Why Globals Should Rethink Drinking
In the Global, drinking alcohol is often part of social gatherings, celebrations, and even stress relief. But beyond the headache and hangover lies a more serious risk: alcohol is a known carcinogen; it can cause cancer.
Whether you drink occasionally or regularly, research shows that even small amounts of alcohol can increase your risk of developing several types of cancer.
This article explains how alcohol affects your body, what cancers are linked to alcohol, and how Globals can reduce their cancer risk without giving up their social life entirely.
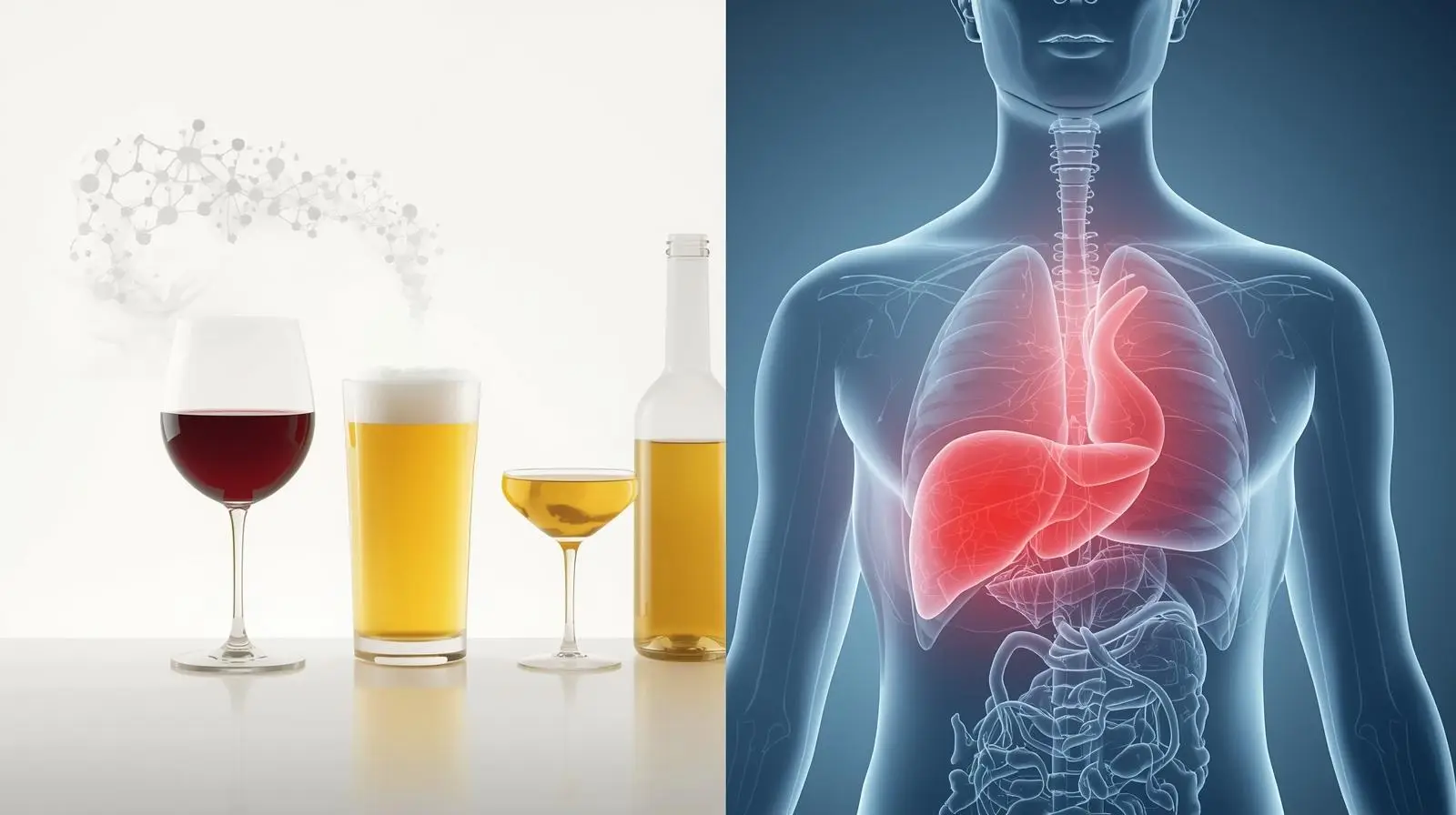
What Happens When You Drink Alcohol?
Every time you consume beer, wine, or spirits, your body goes to work breaking down the ethanol, the active ingredient in alcohol.
This process primarily occurs in the liver, where enzymes convert ethanol into acetaldehyde, a highly toxic and carcinogenic compound.
Acetaldehyde is dangerous because:
- It damages DNA inside cells, making it harder for your body to repair mutations.
- It disrupts normal cell function, leading to cell mutations and uncontrolled growth.
- It causes oxidative stress and chronic inflammation, weakening the immune system’s ability to detect and destroy cancer cells.
Even small amounts of alcohol can trigger this toxic process. That’s why alcohol causes cancer not only at high doses but even with moderate consumption, according to the National Cancer Institute and Cancer Research UK12.
Additionally, alcohol:
- Increases estrogen levels, which is why it’s linked to breast cancer.
- Weakens nutrient absorption (especially folate), a vitamin that protects cells from mutations.
- Enhances the absorption of carcinogens from tobacco smoke when drinking and smoking are combined.
Which Cancers Are Linked to Alcohol Use?
Extensive research has shown that alcohol consumption increases the risk of at least seven significant types of cancer. These are not based on myths; they are documented by global health authorities, such as the International Agency for Research on Cancer (IARC) and the World Health Organization (WHO).
1. Mouth, Throat, and Esophagus Cancer
- These cancers are strongly linked to alcohol, especially when combined with smoking.
- Alcohol makes the tissues in the mouth and throat more permeable, allowing carcinogens to penetrate deeply.
2. Liver Cancer
- Long-term alcohol use causes liver inflammation, scarring (cirrhosis), and impaired detoxification.
- A damaged liver is more likely to develop hepatocellular carcinoma (HCC), the most common form of liver cancer.
In the Global, liver cancer is one of the top causes of cancer death, alcohol and hepatitis B/C co-infection make it worse.
3. Breast Cancer (in Women)
- Alcohol increases levels of estrogen and other hormones, which fuel the growth of hormone-sensitive breast tumors.
- Even just one drink per day has been shown to raise breast cancer risk in women by 7–10%2 %.
4. Colorectal (Colon and Rectal) Cancer
- Alcohol irritates the lining of the colon and rectum and disrupts gut bacteria.
- It interferes with folate metabolism, a nutrient that helps protect DNA from damage.
5. Stomach and Pancreatic Cancer
- Chronic alcohol intake increases stomach acidity and inflammation, leading to damage to the stomach lining.
- It is also associated with an increased risk of pancreatic cancer, especially in combination with other risk factors like smoking and obesity.
Summary Table: Alcohol-Linked Cancers
| Cancer Type | How Alcohol Increases Risk |
| Mouth, Throat, Esophagus | Damages the cell lining, enhances tobacco carcinogen entry |
| Liver Cancer | Causes cirrhosis and liver inflammation |
| Breast Cancer | Increases estrogen levels |
| Colon and Rectal Cancer | Disrupts digestion, affects folate levels |
| Stomach & Pancreatic Cancer | Triggers chronic inflammation |
How Much Alcohol Raises Cancer Risk?
There’s No “Safe” Level
Many Globals believe that moderate drinking is harmless. But multiple studies show that there’s no completely safe level of alcohol when it comes to cancer risk.
Risk increases with every additional drink, even at “moderate” levels.
| Drink Type | Standard Serving in PH | Cancer Risk Level |
| Beer (330 ml) | 1 bottle | Mild to moderate |
| Wine (150 ml) | 1 glass | Moderate |
| Spirits (40 ml shot) | 1 shot | Moderate to high |
Who Is at Higher Risk?
Genetics + Alcohol = Dangerous Mix
Some Globals have a genetic trait called ALDH2 deficiency, which causes alcohol flushing (red face after drinking).
This trait makes it harder to break down acetaldehyde, leading to higher levels of toxins in the body and a much greater risk of esophageal and head & neck cancers.
Other high-risk groups include:
- Those with a family history of cancer
- Smokers and people exposed to secondhand smoke
- Individuals with liver problems or hepatitis B/C
Alcohol + Smoking = Double Trouble
If you smoke and drink, your cancer risk doesn’t just add up, it multiplies.
According to Cancer Research UK, smokers who also drink alcohol are several times more likely to develop mouth, throat, or esophageal cancer than those who do neither.
This is especially relevant in the Global, where both drinking and smoking are common among men.
Common Myths About Alcohol and Cancer
| Myth | Fact |
| Red wine is good for the heart, so it must be safe. | Red wine still contains ethanol, the cancer-causing ingredient. |
| Beer is less harmful than hard liquor. | All alcohol types increase cancer risk—it’s the ethanol, not the drink. |
| I only drink on weekends. | Binge drinking causes high toxic exposure, even if done infrequently. |
Can Quitting Alcohol Reverse Cancer Risk?
Good News: It’s Never Too Late
Even if you’ve been drinking for many years, quitting or reducing alcohol consumption can significantly lower your cancer risk, and your body begins to heal faster than you might think.
According to the National Cancer Institute and multiple global studies, people who stop drinking alcohol gradually reduce their risk of developing alcohol-related cancers, especially in the mouth, throat, liver, breast, and colon1.
Quitting alcohol gives your body a chance to repair cellular damage, restore immune function, and reduce chronic inflammation, all of which are key drivers of cancer.
Here’s how your body responds after cutting back:
After 1 Year
- DNA damage starts to decrease. The levels of acetaldehyde (the toxic chemical produced from alcohol) drop dramatically.
- Liver function improves, especially in those with early-stage liver disease or fatty liver caused by alcohol.
- Your body’s detoxification system functions more effectively, which may help reduce the accumulation of cancer-promoting substances.
After 5 Years
- The risk of mouth, throat, and esophageal cancers begins to decline, especially if you also stop smoking.
- Cell turnover normalizes, meaning new healthy cells are less likely to mutate or become cancerous.
- Your digestive and immune systems stabilize, allowing the body to fight inflammation and early abnormal cell growth better.
Long-Term (10+ Years)
- The risk of breast cancer in women and colorectal cancer continues to decrease, especially with a healthy lifestyle.
- Overall, the risk of cancer mortality declines as the body regains its ability to protect and repair itself at the cellular level.
- When combined with good nutrition, regular physical activity, and routine health check-ups, the protective benefits of alcohol cessation are even greater.
The Global Picture: Alcohol and Cancer in the Global
- According to a 2021 DOH survey, 6 out of 10 Global adults consume alcohol at least once a month.
- Breast and liver cancer are the top 5 cancers in the country, both linked to alcohol.
- Despite this, awareness of alcohol’s cancer risk is very low, especially among women.
Philippine health policy lacks strong warning labels on alcohol products. Unlike tobacco, alcohol marketing remains widely visible and under-regulated.
Final Takeaway: Know the Risk, Choose Wisely
Alcohol is officially classified as a Group 1 carcinogen—the same category as tobacco and asbestos. While it’s socially accepted and often glamorized, its link to cancer is scientifically proven and serious.
Key Messages:
- There’s no truly safe level of alcohol when it comes to cancer.
- Reducing alcohol intake, even by a few drinks a week, lowers your risk.
- Stay informed, share the facts, and make healthy choices for your future.
Always consult your doctor or healthcare provider if you’re concerned about your cancer risk or alcohol use. Early awareness saves lives.
References
- National Cancer Institute. Alcohol and Cancer Risk. Click here
- Cancer Research UK. Alcohol and Cancer. Click here
- MD Anderson Cancer Center. Alcohol and Cancer Risk Advisory. Click here
- PubMed: Brooks, P. J., et al. (2009). Acetaldehyde and DNA damage in ALDH2-deficient populations. Click here